Introduction
Now, I’m not here to scare you. But there are many conditions out there that are so uncommon we often don’t even know that they exist. Unfortunately, sometimes these conditions may walk into our clinics and have us shaking our heads in disbelief and asking ourselves… ‘why don’t you fit into that diagnosis!’. I think, for many, pigmented villonodular synovitis (PVNS) of the knee is one of these diagnoses. It is quite rare, however, it presents similarly to many of the conditions that we as sports physiotherapists treat on a daily basis. This article discusses PVNS including assessment, diagnosis, and the treatment options.
Background Information
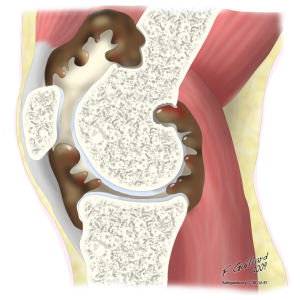
Pigmented villonodular synovitis of the knee is a proliferative and inflammatory condition of the synovial tendon in the joint, tendon sheath or bursa. This disease can be disabling and is characterised by a proliferation of synovial tissue (Ottoviani, 2011). Thus, it is a slow growing, albeit benign, locally invasive tumor of the synovium.
Fortunately, the condition is quite rare with an estimated incidence of 1.8 per 1,000,000 (Myers & Masi, 1980). However, this is something that you should be on the look out for! The most commonly affected age group is 20 to 60 year olds. Thus, there is the potential for this to occur in your adult athletes and someone with this condition may walk in your doors.
Classification of Pigmented Villonodular Synovitis
There are two forms of pigmented villonodular synovitis of the knee (Ofluoglu, 2006):
- Diffuse: when 1 compartment or entire synovium of a joint is affected. This is the more common type, and usually affects the larger joints (the hip and the knee)
- Localised/Nodular: usually occurs in smaller joints and when a single mass is affected
Diffuse PVNS of the knee is the most common presentation, accounting for up to 80% of presentations (Ottoviani, 2011).
Diagnosis of Pigmented Villonodular Synovitis of the Knee
As is the case with many conditions, your objective findings will depend on a few things including:
- Form of PVNS i.e. diffuse or localised/nodular
- Progression of the disease
- Location of the synovitis/tumor
It is difficult to make an early diagnosis, with an average delay in diagnosis of 4.4 years (Bhimani et al., 2001).
Subjective Assessment
Ottoviani et al (2011) reviewed 122 cases of PVNS and identified the most common features of clinical presentation. They suggested that those with PVNS are likely to report:
- Joint Pain (80%). Often presents as a deep joint ache.
- Swelling (79%)
- Mechanical Symptoms (clicking, locking and even instability) may be present in those with nodules of tissue affecting the weight bearing surfaces.
- Mechanism: the patients rarely reported a definitive mechanism (useful for differentiation of diagnoses). They will often present with swelling and joint pain with no apparent cause, and this may have occurred a number of times over previous years (Bhimani et al., 2001).
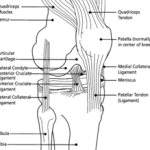
Objective Assessment
Patients with PVNS may present with:
- Reduced and painful ROM
- Positive Swipe Test for effusion. Haemarthrosis is present in approximately 75% of cases (Ottiviani et al., 2011)
- There is potential for a palpable nodule (dependent upon location of lesion)
- Joint line tenderness
- As may be expected; ligamentous testing will be negative
Imaging Assessment
The gold standard of imaging for diagnosis
X-Ray
- Radiographic findings of diffuse intra-articular PVNS are normal in up to 21% of cases (Murphey et al., 2008)
- Abnormal radiographs will display joint effusion, soft tissue swelling, absence of calcification, extrinsic erosion of bone, preservation of joint space, and normal bone mineralization
- The most useful form of imaging; and is often the key element for diagnosis (Ottoviani et al., 2011).
- Common features include proliferative synovitis, synovial thickening, and villous or nodular projections (Murphey et al., 2008)
Differential Diagnoses
There are a few differential diagnoses that you should be aware of, these include:
- Rheumatoid arthritis
- Meniscal injury
- Patellofemoral pain:
- Osteoarthritis
The astute clinician will note the differences between the presentation of PVNS and the above differential diagnoses.
Conservative Physiotherapy Management
Conservative management is not indicated in the case of pigmented villonodular synovitis of the knee, as it will ultimately fail. Therefore, early diagnosis is beneficial so that an appropriate referral to a orthopaedic specialist may occur.
Surgical Management of Pigmented Villonodular Synovitis
There are a few surgical options for the management of PVNS and again it depends on the characteristics of the disease. The preferred options for PVNS of the knee are:
- Synovectomy via Arthroscopy
- Synovectomy via Arthrotomy
- Total Knee Replacement: indicated when there is significant joint destruction
- Complementary therapies include: radiotherapy and isotopic synoviorthesis. The value of these complementary therapies is unknown.
Outcomes Following Surgery
Despite what may be seen as “radical” treatment, there is a high relapse rate following surgery of 25-55% (Akinci et al., 2011; Ottoviani et al, 2011). In the small long-term follow-up study by Akinci et al. (2011) 89.5% of patients had either a good or perfect score on the Knee Society Score at an average of 80 months following surgical intervention. It is worth noting that 7 out of the 19 patients did however progress to a total knee replacement, demonstrating that this destructive condition leads to early osteoarthritic change.
Clinical Implications and Take Home Messages
- This is a rare condition, however, there is the real possibility of this ‘walking’ into your clinic
- Diagnosis is challenging, and frequently delayed. So keep your eyes and ears open
- This condition may present similarly to other more common conditions, but there will be some hallmark differences
- Conservative management will ultimately fail
- Surgical management is indicated, although chance of relapse and early onset osteoarthritis is high
- There is a dearth of quality research on this condition
- Diagnose this early, and earn some serious respect from all involved
What Are Your Thoughts?
Have you ever seen or heard of this condition? I would love to hear your input, so be sure to let me know in the comments or catch me on Facebook or Twitter. Are you a physiotherapist or physical therapist looking to promote your own clinic, check this out.
Photo Credit: compujeramey
References
Akinci O, Yavuz A, Incesu M, Eren A. Long-term results of surgical treatment of pigmented villonodular synovitis of the knee. Acta Orthop Traumatol Turc 2011;45(3):149-155
Bhimani MA, Wenz JF, Frassica FJ. Pigmented villonodular synovitis: keys to early diagnosis. Clinical Orthopaedics and Related Research 2001;386:197-202.
Murphey MD, Rhee JH, Lewis RB, Fanburg-Smith JC, Flemming DJ, Walker EA. Pigmented Villonodular Synovitis: Radiologic-Pathologic Correlation. RadioGraphics 2008;28:1493–1518
Myers BW, Masi AT. Pigmented villonodular synovitis and tenosynovitis: a clinical epidemiologic study of 166 cases and literature review. Medicine (Baltimore) 1980;59(3):223-38.
Ofluoglu O. Pigmented villonodular synovitis. Orthop Clin North Am 2006;37(1):23-33
Ottaviani S, Ayral X, Dougados M, Gossec L. Pigmented villonodular synovitis: A retrospective single-center study of 122 cases and review of the literature. Semin Arthritis Rheum 2011;40:539-546
Related Posts







I have had arthroscopic surgery on my left knee but still have problems. My doctors and I now believe I have pvns. We are exploring treatments both surgery and radiology. Can you please give me some more info on treatment or doctors that have some experience treating pvns? Thank you.
Barry
I was diagnosed with pvns back in 1998. I had arthroscopic surgery and was advised that it would come back and it did within six months. Since then I have lost almost all range of motion in my right leg. To this day I live with the swelling, popping,cracking and pain in my knee to the point I have to use about 1200 mg of ibuprofen five times a day. My doctor has aspirated it several times and has been astounded by the amount of fluid he has taken off my knee. I miss being able to run and kick a soccer ball around with my kids. Would a total knee replacement be in my best interest?