Introduction
Many sports physiotherapists rehabilitate hamstring injuries on a daily basis. This is not hard to fathom when you recognise in some sports, such as Australian Football, hamstrings injuries are the most common of any injury (Warren et al., 2010). Unfortunately, when they do occur they can be very tricky to fully and definitively rehabilitate fully and reported re-injury rates are as high as 50% (Askling et al., 2003). This statistic inevitably leads to the people screaming it is due to inadequate rehabilitation techniques, which may be correct (Orchard & Best, 2002). Accordingly, this article will discuss new research which compares the clinical and morphological effects of 2 effective rehabilitation programs for hamstring injuries (Slider et al., 2013).
Background Information
Given its high incidence in many sports, hamstring injuries have been widely studied. Whilst I feel we don’t know anywhere near as much as we need, there is plenty already known about hamstring injury rehabilitation. The goals of any muscle strain rehabilitation program are to promote muscle tissue healing and enhance functional performance, which should correlate to important outcomes such as expedited return to play, improved athletic performance, and reduced risk of re-injury.
When considering reduction of hamstring injury risk there has been previous support for multiple interventions, including:
- Neuromuscular control exercises (Cameron et al., 2009)
- Eccentric training (Askling et al., 2003; Petersen et al., 2011)
- Progressive Agility and Trunk Stabilisation (PATS) (Sherry & Best, 2004)
Accordingly, it has been suggested that these interventions should be included as part of a rehabilitation program following acute strain. However, until recently there has been no direct comparison of the PATS and eccentric strengthening programs in terms of restoration of hamstring muscle integrity and function. Take us to the new research…
Hamstring Injury Rehabilitation Programs
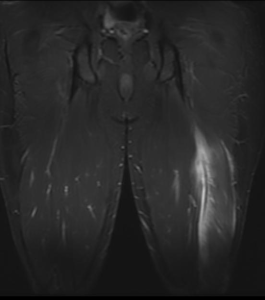
Slider et al (2013) performed an equal-randomised, double-blind, parallel-group study to determine the differences in clinical and MRI outcomes following two different rehabilitation programs. 29 participants underwent a 4-block, fixed-allocation randomisation process to assign subjects to 1 of the 2 rehabilitation groups i.e. the Progressive Agility and Trunk Stabilisation (PATS) or Progressive Running and Eccentric Strengthening (PRES). The authors of the study assessed the following outcomes:
- Return to sport (days)
- MRI was performed at randomisation and completion of rehabilitation. This assessed cranio-caudal length, cross-sectional area and location of injury
It was assumed that the 2 differing programs would produce some differences in the above outcomes. The rehabilitation programs utilised are discussed below.
Progressive Running and Eccentric Strengthening Program
This rehabilitation program was based on a program utilised by Baquie and Reid (1999). For the full program I recommend you access the cited article here. However, as a short indication, the program is based on 3 phases:
- Phase 1: short-stride jogs and hamstring isometric exercises.
- Phase 2: concentric and eccentric strengthening exercises. Running with progressive acceleration/deceleration
- Phase 3: intense eccentric strengthening with a power component. Sprinting with progressive acceleration/deceleration
Phase 2 Exercise Example – Prone Hamstring Curl
Phase 3 Exercise Example – Nordic Hamstring Curl
Progressive Agility and Trunk Stabilisation Program
The PATS rehabilitation program was a modified version of the program previously utilised by Sherry and Best (2004). Again, for the full program I recommend you access the cited article here. This program, too, was based on 3 phases:
- Phase 1: movements in frontal and transverse plane e.g. side shuffles and grapevines for agility and side planks
- Phase 2: agility and trunk stabilisation movements in the transverse and sagittal planes e.g. boxer shuffles, rotating body bridges
- Phase 3: increased the speed and/or resistance of the exercises e.g. forward/back accelerations, walking lunges with rotations
Phase 1 Exercise Example – Bent Knee Bridge
Phase 2 Exercise Example – Rotating Body Bridges
Return To Play Assessment
The athletes were allowed to return to sport when they had:
- No palpable tenderness along the posterior thigh
- Subjective readiness (no apprehension) after completing a series of progressive sprints working up to full speed
- 5/5 on manual muscle testing of the hamstrings performed on 4 consecutive repetitions in various knee positions (prone lying with knee flexed at 90° and 15° then testing with tibia in neutral, ER and IR).
So What Were The Results?
Following randomisation there were no significant differences between groups for initial MRI or physical examination measurements. Following intervention the authors found the following results:
- Return To Sport Timeframes: The mean time to return to sport was 28.8 in the PRES group and 25.2 in the PATS group
- CC Length: At return to sport, CC length in the PRES group was 15.9 cm compared to 7.9 cm in the PATS. However, this is likely the result of edema drainage into the fascial plane that occurs during rehabilitation, which extends beyond the site of soft tissue damage.
- The PRES athletes displayed less improvement in injury CC length with an average improvement from baseline of 1.4 cm compared to 5.0 cm for those in the PATS
- There were no significant differences in clinic visits or rehabilitation compliance
- Re-injury rates were low in both groups, 1 in PATS and 3 in the PRES, discussed further below.
Limitations of Research
There are a number of limitations to this research, many of which the authors are fully aware. These include:
- Small sample size
- High drop out percentage
- As previously discussed, it is not feasible for most recreational athletes to obtain MRI following injury.
- Questionable return to play assessment (discussed further below)
- Questionable return to sport definition (discussed further below)
Return to Sport Definition
When referring to “return to sport”, the authors used the period from injury to completion of rehabilitation rather than return to competition or pre-injury level of performance. This meant that the results of this study allowed for much quicker median “return to play” (23 days) than previous studies (112 days) (Askling et al., 2007). Seems a big difference doesn’t it, and quicker than what is often seen clinically!
Return to Play Assessment
Another factor that may explain the significant differences in return to play times is the return to play assessment (criteria for RTP is discussed above). Firstly, isometric manual muscle testing was utilised to assess for hamstring strength deficits. Whilst this is clinically replicable, previous research has suggested the sensitivity to differences between sides and to deficits relative to normal is less than 75% (Bohannon, 2005). Secondly, the article suggests that 11 athletes were allowed to complete rehabilitation and return to play despite ongoing hamstring symptoms (ie. pain and tightness). Finally, it was suggested that there were differences or deficits of hamstring flexibility in some athletes.
Interestingly, the PRES athletes showed greater range of motion during the straight leg raise in the non-injured limb while the PATS had reduced ROM (whilst it may not have impacted this situation, eccentric training has been shown to improve flexibility). The ongoing hamstring deficits are displayed by the finding that at 3, 6, 9, and 12 month follow-ups between 2 and 5 subjects reported continuing hamstring symptoms.
Confusingly, despite what may be considered a non-comprehensive assessment, which may have allowed for an earlier RTP from injury, the re-injury rate in the study was lower than many previously recorded. Only 4 subjects of 29 randomised reported a hamstring re-injury; 2 occurred during rehabilitation phase and 2 after the completion of rehabilitation. This may have been due to the study population i.e. non-professional athletes. It is likely that the study subjects competed at a lower intensity upon RTP, particularly given the ongoing symptoms in multiple subjects.
Clinical Implications of This Research
This article both produced some interesting results and confirmed some notions we already knew. These include:
- Initial CC length of injury was significantly associated with a longer return-to-sport time, supporting previous research (Askling et al., 2007; Connell et al., 2004)
- Despite successful RTP – MRI displayed ongoing signs of healing following hamstring injury
- The two differing rehabilitation programs produced no significant differences in return-to-sport time, clinic visits, or rehabilitation compliance
Final Thought: As we stated in the post of preventing hamstring injuries, interventions to prevent hamstring injury should be as individualised as the athlete themselves… and treatment/rehabilitation is certainly no different.
What Are Your Thoughts?
What are your experiences when rehabilitating hamstring injuries? I would love to know, so be sure to let me know what you think of this new research in the comments or you could:
Promote Your Clinic: Are you a physiotherapist or physical therapist looking to promote your own clinic? Check this out.
References
Askling C, Karlsson J, Thorstensson A. Hamstring injury occurrence in elite soccer players after preseason strength training with eccentric overload. Scand J Med Sci Sports. 2003;13:244-250.
Askling C, Saartok T, Thorstensson A. Type of acute hamstring strain affects flexibility, strength, and time to return to pre-injury level. Br J Sports Med. 2006;40:40-44.
Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. Am J Sports Med. 2007;35:197-206.
Baquie P, Reid G. Management of hamstring pain. Aust Fam Physician. 1999;28:1269-1270.
Bohannon RW. Manual muscle testing: does it meet the standards of an adequate screening test? Clin Rehabil 2005;19(6):6662-667
Cameron ML, Adams RD, Maher CG, Misson D. Effect of the HamSprint Drills training programme on lower limb neuromuscular control in Australian football players. J Sci Med Sport. 2009;12:24-30
Connell DA, Schneider-Kolsky ME, Hoving JL, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. AJR Am J Roentgenol. 2004;183:975-984.
Orchard J, Best TM. The management of muscle strain injuries: an early return versus the risk of recurrence. Clin J Sport Med. 2002;12:3-5.
Petersen J, Thorborg K, Nielsen MB, Budtz- Jørgensen E, Hölmich P. Preventive effect of eccentric training on acute hamstring injuries in men’s soccer: a cluster-randomized controlled trial. Am J Sports Med. 2011;39:2296-2303.
Sherry MA, Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. J Orthop Sports Phys Ther. 2004;34:116-125
Slider A, Sherry MA, Sanfilippo J, Tuite MJ, Hetzel SJ, Heiderscheit BC. Clinical and Morphological Changes Following 2 Rehabilitation Programs for Acute Hamstring Strain Injuries: A Randomized Clinical Trial. J Orthop Sports Phys Ther 2013;43(5):284-299
Warren P, Gabbe BJ, Schneider-Kolsky M et al. Clinical predictors of time to return to competition and of recurrence following hamstring strain in elite Australian footballers. Br J Sports Med 2010 44: 415-419
Photo Credit: Ronnie Macdonald, Dr Roberto Schubert
Related Posts