Introduction
In the sports physiotherapy world we are frequently called upon to assess and treat athletes of all ages. As you might expect, this may range from young children through to nonagenarian Master’s athletes. Sports physiotherapists would know when dealing with young athletes missing a career-ending (yes, career) diagnosis can be unforgivable. One such diagnosis is juvenile osteochondritis dissecans of the knee, a condition that commonly affects athletic children, and one that if left unchecked could jeopardise the integrity of their knee. Thus, accurate and timely diagnosis followed by appropriate management is essential when dealing with juvenile osteochondritis dissecans.
Background Information
Osteochondritis dissecans is an acquired, potentially reversible, idiopathic lesion of the subchondral bone resulting in delamination and sequestration, with or without articular involvement and instability. (Kocher et al., 2006.)
Whilst its title is a misnomer, as it wrongly implies an inflammatory condition and should be more appropriately termed ‘osteochondrosis’, the original name has stuck. It refers to a condition with an incidence of 15 – 29 per 100 000 (Kocher et al., 2006). The condition is seem most commonly in children, and growing participation by children in competitive sports at younger ages has meant that the mean age of onset of osteochondritis dissecans is decreasing. There is a definite gender bias, with males predominately affected at a ratio of 5:3 (Cahill, 1995). The condition is seen bilaterally in up to 25% of individuals (Schenk & Goodnight, 1996). As previously mentioned, if left unchecked this condition may jeopardise the joint and lead to early onset osteoarthritis.
Aetiology of Osteochondritis
Whilst osteochondritis dissecans may in theory affect an joint, 65-75% of cases are seen in the knee, 70% of which are found to affect the postero-lateral aspect the medial femoral condyle (Schindler, 2007). There has been many postulated causes of OCD, including:
- Inflammation
- Genetics
- Ischaemia
- Ossification
- Repeated Micro-trauma
However, there remains insufficient evidence to conclusively definitively support these causes (Kocher et al., 2006). If you are interested in the individual merits of each hypothesis I would point you to the article by Schindler (2007), who discusses each in depth. Currently, the most widely accepted cause is the influence of repeated micro-trauma. Authors suggest that repetitive trauma induces a stress reaction resulting in a stress fracture within the underlying subchondral bone. When and if this loading persists, thus exceeding the ability of the subchondral bone to heal, necrosis of the fragment may occur, leading to fragment dissection, separation, and finally nonunion (Kocher et al., 2006)..
Classification of Juvenile Osteochondritis Dissecans of the Knee
So much to classify, so little time. As previously stated, osteochondritis dissecans most commonly affects children, however, it can also affect adolescents and even adults. Osteochondritis dissecans can be classified by the maturation status of the distal femoral physis:
- Juvenile Osteochondritis Dissecans: those with a wide open physis
- Adolescent Osteochondritis Dissecans: those with a closing physis
- Adult Osteochondritis Dissecans: those with a closed physis.
As stated previously, this article will focus on juvenile osteochondritis dissecans (the most common form). There are many different classification systems that are used for juvenile osteochondritis dissecans. Two popular classification or staging systems are shown below. The first is presented by Hefti et al (1999) and is based on MRI findings:
- Stage 1: Small change without clear margins of fragement
- Stage 2: Osteochondral fragment with clear margins but without fluid between fragment and underlying bone
- Stage 3: Fluid is visible partially between fragment and underlying bone
- Stage 4: Fluid is completely surrounding the fragment, but the fragment is in situ.
- Stage 5: Fragment is completely detached and displaced (loose body).
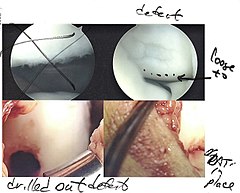
The second is Guhl’s (1982) classification and is based on findings of arthroscopic assessment:
- Stage I: Intact Lesions
- Stage II: Lesions showing signs of early seperation
- Stage III: Partially detached lesions
- Stage IV: Craters with loose bodies.
The stage of osteochondritis will likely affect your subjective findings, objective findings and also the course of management undertaken.
Subjective Assessment
The patient that presents with juvenile osteochondritis dissecans may report the following:
- Pain or discomfort antero-medial to the patella (think: classic OCD lesion on the medial femoral condyle)
- However, pain is frequently nonspecific and includes poorly localized
- Symptoms are exacerbated by exercise, particularly when climbing hills or stairs.
- Mechanism: patients rarely report a specific mechanism
- Patient may report swelling and stiffness
- Mechanical symptoms, such as locking or catching, are common in later stage OCD and indicate unstable, loose fragments (Guhl Stage III and IV)
Objective Assessment
Your objective assessment may uncover the following information:
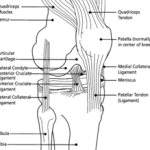
- Observation: an effusion may be visible. Quadriceps wasting may suggest longer presence of symptoms
- Gait: an analgic gait, with tibial external rotation may be present
- Palpation: maximal tenderness can often be elicited over the antero-medial aspect of the knee with varying amounts of knee flexion (again think: classic OCD lesion on the medial femoral condyle). This is called a positive Axhausen’s sign (Axhausen, 1922).
- Wilson’s Sign: pain with internal rotation of the tibia. Unfortunately, the Wilson sign lacks sensitivity (75% of patients with OCD were found to have a negative result) (Conrad and Stanitski, 2003).
- Swipe Test: useful for the detection of an effusion.
Imaging for Osteochondritis Dissecans
Radiographic information is essential if there is a clinical suspicion of osteochondritis dissecans. It is important for:
- Confirmation of diagnosis
- Lesions characterisation
- Predicting prognosis
- Making informed management decisions
- Assessing recovery and healing during treatment.
X-Ray
Plain radiographs can be used in both children and adults to rule out other bony injury, evaluate skeletal maturity, characterise and localise the OCD lesion and indicate its age. The following view should be taken:
- AP
- Lateral
- Notch views (for imaging the posterior femoral condyles)
- Skyline (if patellar involvement is suspected)
Magnetic Resonance Imaging
MRI should be considered a normal part of the diagnostic evaluation, as it can accurately assess:
- The lesion size and status
- Status of cartilage and subchondral bone
- Bony oedema
- The presence of any loose bodies
All of this information provides a rough guide to prognosis, as smaller lesions with intact cartilage are much more likely to respond to non-operative treatment, especially in skeletally immature (juvenile) patients (Kocker et al., 2006).
Conservative Physiotherapy Management of Osteochondritis Dissecans
There is widespread agreement that initial non-operative management is indicated in juvenile osteochondritis dissecans (Schindler, 2007; Kocher et al., 2006). Cahill (1995) has previously reported that 50% of juvenile OCD lesions will heal within a 10- to 18-month period provided the physis remains open and patient compliance is maintained (which is at times very difficult!!). Whilst there is some controversy in the literature regarding immobilisation time-frames (think: the role of mobilisation for joint and cartilage health), there is some consensus on a general 3 phase management protocol. It is outlined below.
Phase 1 (Weeks 0 – 6)
- Knee immobilisation (cast or brace)
- PWB with crutches
- Criteria for Progression: child must be pain free
Phase 2 (Weeks 6 – 12)
- Out of brace/cast
- WBAT
- Commencement of rehabilitation: knee ROM and low impact strengthening (quads, hams). Sports still restricted
- Criteria for Progression: clinical and radiographic signs of healing.
- Graduated return to loading: running, jumping and eventually sports.
- Complete absence of knee symptoms is required to increase intensity.
- Repeat MRI provides valuable information on lesion healing.
Surgical Management of Osteochondritis Dissecans
There are a few indications for surgical management. These are:
- Skeletally immature patients with detached or unstable lesions
- Failure of non-operative management
- Adult patients
The goals of surgical management are (Smillie, 1957):
- Maintenance of joint congruity
- Allow healing of the junctional subchondral bone
- Rigid fixation of unstable fragments
- Repair any osteochondral defects
- Drilling: antegrade and retrograde
- Internal Fixation
- Abrasion and Microfracture
- Osteochondral Autograft Transplantation
- Osteochondral Allograft Transplantation
- Autologous Chondrocyte Implantation
As you might expect there are various indications and success rates for each of these surgeries. If you are interested in more information, I would point you to this fantastic article (PDF): Surgical Treatment Options for Osteochondritis Dissecans of the Knee. It includes a great algorithm which orthopaedic surgeons may use to assist in decision making.
Clinical Implications and Take Home Messages
- This is a condition which commonly affects young athletic populations
- Clinical diagnosis can be challenging, so you should maintain a high clinical suspicion of this condition
- Imaging is an important diagnostic tool and not to be shied away from.
- In juvenile osteochondritis dissecans conservative physiotherapy management is the first port of call
- There are many surgical options available should conservative management fail
What Are Your Thoughts?
I would love to hear about your experiences dealing with osteochondritis dissecans? Do you find it particularly challenging? What has helped you in the management of this condition? Help us all out and let me know in the comments below, or hit me up on Facebook or Twitter.
References
Cahill BR. Osteochondritis dissecans of the knee: treatment of juvenile and adult forms. J Am Acad Orthop Surg. 1995;3:237-247.
Conrad JM, Stanitski CL. Osteochondritis dissecans: Wilson’s sign revisited. Am J Sports Med. 2003;31:777-778.
Ewing JW, Voto SJ. Arthroscopic surgical management of osteochondritis dissecans of the knee. Arthroscopy. 1988;4:37-40
Garrido CP, McNicke AG, Cole BJ. Surgical treatment options for osteochondritis dissecans of the knee. Sports Health 2009;1(4):326-334.
Guhl JF. Arthroscopic treatment of osteochondritis dissecans. Clin Orthop Relat Res. 1982;167:65-74.
Hefti F, Beguiristain J, Krauspe R, et al. Osteochondritis dissecans: a multicenter study of the European Pediatric Orthopedic Society. J Pediatr Orthop B. 1999;8:231-245.
Kocher MS, Tucker R, Ganley TJ, Flynn JM. Management of osteochondritis dissecans of the knee. American Journal of Sports Medicine 2006;34(7):1181-1191.
Schenk Jr RC, Goodnight JM. Osteochondritis dissecans. JBJS 1996;78-A:439–56.
Schindler OS. Osteochondritis dissecans of the knee. Current Orthopaedics. 2007;21:47-58.
Smillie I. Treatment of osteochondritis dissecans. J Bone Joint Surg Br. 1957;39:248-260
Related Posts
Comments










tanks….sir
It helps me to enhance my knowledge thanks