Introduction
I don’t think anyone would disagree that wrist presentations are less common in clinical physiotherapy practice. So how would you like me to double up on the rarities, by discussing a rare wrist presentation? Well, I’m going to anyway. Kienbock’s Disease is a rare and infrequently discussed source of dorsal wrist pain that you could definitely encounter in your clinical practice. The condition is named after the Viennese radiologist Robert Kienbock who presented his findings on the disorder in his 1910 publication ‘Concerning traumatic malacia of the lunate and its consequences’. This condition, discussed in depth below, primarily affects people between 15 and 40 years old and has been documented in athletes from many sports that include repetitive use of the wrist e.g. golf, tennis, martial arts, etc (Nakamura et al., 1991). Therefore, if you work with athletes from these sports, you should remain on high alert for the occurrence of Kienbock’s disease.
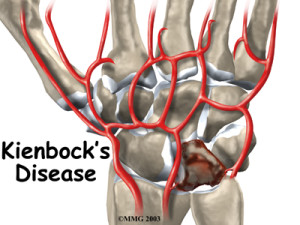
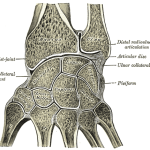
Pathoanatomy of Kienbock’s Disease
Kienböck’s disease, or lunatomalacia as it is sometimes referred to, is an aseptic osteonecrosis of the lunate bone initiating a progressive collapse of the lunate bone, followed by total carpal collapse (Smet & Degreef, 2009). It was the original view of Kienbock that:
“This condition is due to a disturbance in the nutrition of the lunate caused by the rupture of ligaments and blood vessels during contusion, sprain, or subluxation’’ (Peltier, 1980).
Whilst this view is widely supported, it has been suggested that Kienbock’s disease is a disorder of multifactorial aetiology causing avascular necrosis. As an example, Hulten (1928) suggested ulnar-minus variance was a predisposing factor for the development of Kienbock’s, however, this theory has recently been refuted by detailed studies of ulnar variance (Lichtman et al., 1977). Regardless, it is commonly agreed that trauma (micro or otherwise) occludes the vessels that supply the lunate.
Studies by Lee (1963) and Gelberman et al. (1980) have suggested that the patterns of arterial supply may predispose certain people to the avascular necrosis that occurs in Kienbock’s Disease. The carpal bones at greatest risk are those with only a single vessel of supply without anastomoses. Gelberman et al (34) stated that all scaphoids, capitates and 8 to 20% of lunates have this vascular pattern. Thus, this percentage of the population are predisposed to the development of Kienbock’s Disease.
Unfortunately for the practitioner, Kienbock’s Disease is slowly progressive with many non-specific signs and symptoms. However, there is a recognised ‘natural history’ or stages of progression that patients who have developed Kienbock’s Disease progress through. This can give the attentive physiotherapist or physical therapist a guide to a correct and definitive diagnosis.
Stages of Kienbock’s Disease
As suggested above, Kienbock’s Disease has progressive stages, and the following is based on the work of Lichtman et al (2010):
- Stage I: Early stages of the disease with patient reporting symptoms similar to a ‘wrist sprain’ i.e. mild exertional pain increased by axial load in extension. As radiographic appearance of the lunate is normal this was originally a clinical diagnosis. However, with advanced imaging techniques we now see bone scintigraphy is positive and MRI may display signs of bone marrow oedema within the lunate.
- Stage II: As the disease progresses, patients may report more persistent pain (including night pain) and signs of synovitis. Radiographically, the lunate exhibits increased density, however lunate size and shape and carpal alignment is maintained.
- Stage III: As patients progress to stage 3 they report more consistent pain, closely resembling early stage degenerative arthritis. Stage 3 has been re-evaluated and is now split into 2 groups.
- Stage IIIA: In this stage, the lunate has collapsed (loss of height), however the scaphoid maintains a normal position relative to the rest of the carpus.
- Stage IIIB: characterised by lunate collapse and rotatory carpal subluxation leading to a scaphoid “ring” sign on radiographic examination. Patients in this stage will likely report mechanical symptoms.
- Stage IV: The condition has progressed to advanced secondary osteoarthritis of the radiocarpal joint, and the patient will report symptoms of wrist stiffness.
Subjective Assessment
As indicated in the progressive stages above, patients with Kienbock’s Disease will report:
- Mechanism: may be unsure or report a period of repeated micro-trauma
- History: may describe an initial period of intermittent wrist pain with exertional activities such as applying repeated loads to an extended wrist prior to more consistent pain (Lichtman et al., 2010).
- Pain: dorsal wrist pain
- Other Symptoms: weakness, restricted motion and mechanical symptoms as the disease progresses
Objective Assessment
Obviously this is dependent upon the stage of the disease, but you may find:
- Observation: swelling/signs of synovitis
- AROM: reduced ranges of motion
- Strength: reduced grip strength, average 66% (Nakamura et al., 1991)
- Palpation: dorsal tenderness, well localized over the dorsal side of the lunate.
- Special Testing: later stages of disease may have a positive Watson’s Test (Lichtman et al., 2010).
Imaging Assessment
As stated previously, imaging findings will depend on the stage of the disease. In Stage I, plain radiographs may be normal. However, bone scan and MRI are likely to show abnormal changes. However, a small percentage of these patients will have a normal MRI if examined very early on. As the disease progresses, a high resolution computed tomography (CT) best visualizes the bony anatomy of the lunate, and should be used to determine the exact stage of disease (Schmitt and Krimmer, 2007). A CT Scan can allows for visualisation of the lunate osteonecrosis, which has implications for management (discussed below).
Conservative Physiotherapy Management of Kienbock’s Disease
In some cases of Kienbock’s Disease there is a role for conservative non-operative management. In early stages of the disease process, prolonged immobilisation is often used to start treatment in an attempt to enhance spontaneous revascularisation of the lunate. This is first-line treatment in children, adult Stage I, and often as a trial in Stage II/IIIA Kienbock’s Disease. The results of conservative management have been mixed, as Kristensen et al (1986) showed good results after short periods of immobilisation, however, this conflicted the results of Mikkelsen and Gelineck (1987) who displayed poor outcomes after non-operative treatment.
Regardless, of the mixed reports conservative management is only indicated in early stage Kienbock’s Disease. As the disease progresses, surgical management is indicated.
Surgical Management of Kienbock’s Disease
An important thing to remember is that the lunate is the keystone of the proximal carpal row. Unfortunately, a simple resection will lead to immediate and severe collapse of the carpus with inevitable secondary osteoarthritis (Smet & Degreef, 2009). Therefore, other surgical techniques are required, which (yep, you guessed it) are dependent upon the stage of the disease. The surgical techniques are:
Stage I Kienbock’s Disease
- Immobilisation
- Capitate Shortening Osteotomy: to unload the lunate and allow spontaneous revascularisation.
- Revascularisation Procedures: including direct revascularisation and indirect methods such as bone grafting.
- As for Stage 1
- Potential correction of ulnar negative variance – including ulna lengthening or radial shortening procedures. This is aimed at minimising shear forces on the lunate.
- Surgical management aimed at restoring joint stability
- Proximal Row Carpectomy
- Joint Arthrodesis, of either the scaphotrapezium–trapezoid or scaphoid–capitate joints, to further unload the lunate.
- Proximal Row Carpectomy
- May require progression to Total Wrist Arthroplasty or Total Wrist Fusion
Outcomes Following Surgery
Given that this condition is rare, there are infrequent reports of athlete’s outcomes following surgery. Furthermore, it is impossible to currently tell which surgical techniques are more effective than the others. Nakamura et al (1991) evaluated 10 patients with sports-related Kienbock’s Disease who had to give up their usual sport due to pain. The athletes underwent various forms of surgical management, including radial shortening, proximal row carpectomy, and radial osteotomy. Follow-up was a mean of 5 years. Of the athletes, 7 out of 10 returned to their respective sport. Of these, 5 athletes reported their pain had improved, but had not completely gone. So… take from that what you will!
Clinical Implications and Take Home Messages
- Kienbock’s Disease is a rare cause of dorsal wrist pain – but you may still encounter it!
- It progresses slowly, so beware the lame progressive wrist presentation!
- Imaging is required to confirm and accurately assess the stage of the disease
- Early days = conservative, later days = surgical management.
- Surgical management has allowed athletes to return to sport
What Are Your Thoughts?
Do you have experience treating athletes with Kienbock’s Disease? What were your experiences? I would love to know, so be sure to let me know in the comments or catch me on Facebook or Twitter.
Promote Your Clinic: Are you a physiotherapist or physical therapist looking to promote your own clinic, check this out.
References
Gelberman RH, Bauman TD, Menon J, Akeson WH. The vascularity of the lunate bone and Kienböck’s disease. J Hand Surg 1980 ; 5-A : 272-278.
Hulten O. Uber anatomische variationen der handgelenk knochen Ein beitrage zur kenntnis der genese zwei versciedener mondbeinveranderunge. Acta Radiol 9: 155-168 1928
Kristensen SS, Thomassen E, Christensen F. Kienböck’s disease – late results by non-surgical treatment. A follow-up study. J Hand Surg 1986 ; 11-B : 422- 425
Lee M. The intraosseous arterial pattern of the carpal lunate bone and its relation to avascular necrosis. Acta Orthop Scand. 1963, 33: 43–55.
Lichtman DM, Lesley NE, Simmons SP. The classification and treatment of Kienböck’s disease: the state of the art and a look at the future. J Hand Surg Euro 2010;35(7):549-554
Lichtman DM, Alexander AH, Mack GR, Gunther SF. Kienböck’s disease – update on silicone replacement arthroplasty. J Hand Surg 1982 ; 7-A : 343-347.
Lichtman DM, Mack GR, MacDonald RI, et al: Kienbock’s disease: The role of silicone replacement arthroplasty. J Bone Joint Surg 59A 899-908, 1977
Mikkelsen SS, Gelineck J. Poor function after non – operative treatment of Kienböck’s disease. Acta Orthop Scand 1987 ; 58 : 241-243.
Nakamura R, Imaeda T, Suzuki K, Miura T. Sports-related Kienbock’s disease. American Journal of Sports Medicine. 19(1):88-91. 1991.
Peltier LF. The classic. Concerning traumatic malacia of the lunate and its consequences: degeneration and compression fractures. Privatdozent Dr. Robert Kienbo¨ ck. Clin Orthop Relat Res. 1980, 149: 4–8
Schmitt R, Krimmer H. Osteonecrosis of the hand skeleton. In: Schmitt R, Ulrich L (Eds.) Diagnostic imaging of the hand. 1st Edn edition. Stuttgart, New York, Georg Thieme Verlag, 2007: 351–64
Related Posts
Comments




interesting topic i came to know. thanks
Whenever i recieved a pt with the Diagnosis of Keinbocks disease ,i was in the delimma of what to do.
As per common sense a wrist splint and some pain relief measures were the most common treatement options.
This article very clearly helps you to understand what you should do ,and if patient is not improving when to refer back to the doctor.
Arwa
Hello. My name is Michael Williams. I am from Spartanburg, SC. I am now 35 years old, and I was diagnosed with Kienbock’s disease in my right wrist early last year after about 3 months of pain that I thought was a minor sprain that was not healing. I wore a thumb spica for about 90 days seeing no improvement, so I then had a radial shortening on July 5th, 2011. Soon after the surgical wounds had healed and I was off the meds, I could see that the surgery had relieved the throbbing pain. However, to this day, it still hurts to use my wrist, it is very stiff, and if I bump the ends of my fingers or bump my hand in a backwards motion, I just feel like going to my knees in tears of pain. Does anyone else have these same problems after a radial shortening, and do you have any suggestions that will help me with my problem. I send you my thanks in advance for any advice or help that you can give me.
Sincerely,
Michael Williams
Hi Michael,
The best advice I can give – seek an opinion from a physical therapist or physiotherapist near you.
Cheers,
TSP.
Hi i have had keinbock disease in my left wrist and had a total wrist fusen just one year ago. Now my other wrist has started giving my pain just like the other one did been to the Docter and waiting to have a MRI scan to see if it is Keinbock disease . Has anyone had this disease in both wrists ?
Hi all had my MRI scan report back confirmed significant trabecular oedema throughout the lunate in keeping with Kienbock s