Introduction
The condition discussed in this article, you will come to find, is quite complex and can be a battle for the physiotherapist and physical therapist. Thoracic outlet syndrome is considered to be a collection of quite diverse syndromes rather than a single entity (Yanaka et al., 2004), and therefore, accurate diagnosis and enlightened treatment decisions can be very challenging. To be definite about things:
“Thoracic outlet syndrome (TOS) is a symptom complex characterised by pain, paresthesia, weakness and discomfort in the upper limb which is aggravated by elevation of the arms or by exaggerated movements of the head and neck” (Lindgren and Oksala, 1995)
This article will discuss the pathoanatomy, classifications, aetiology, assessment, diagnosis and management of thoracic outlet syndrome.
Pathoanatomy of Thoracic Outlet Syndrome
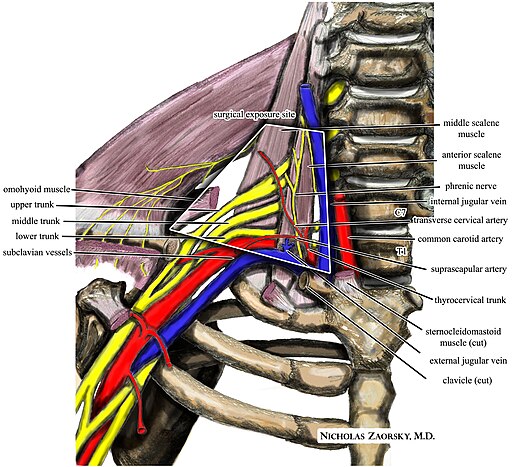
The pain and discomfort of TOS are generally attributed to the compression of the;
- Subclavian vein
- Subclavian artery
- Lower trunk of the brachial plexus
Quite obviously, this will result in a wide variety of symptoms dependent upon the structure that is compressed and the location of compression. In fact, there are three possible sites of compression of the vessels and nerves. These are;
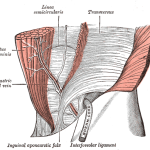
- As they exit from the thoracic cavity and rise up over the first rib and pass between the anterior and middle scalene muscles. This will result in compression of the lower roots of the brachial plexus. It is worth noting that the upper roots of the brachial plexus may also be compressed between the scalene muscles as they exit the cervical spine. However, this condition should technically be referred to as cervical outlet syndrome (Ranney, 1996).
- Beneath the clavicle in the costo-clavicular space, where the neural elements are already outside the thorax (clavicle is removed in the below image).
- In the sub-coracoid tunnel beneath the tendon of the pectoralis minor (removed in the image below) (Wright and Jennings, 2005).
Classification of Thoracic Outlet Syndrome
As suggested previously, there are different types of thoracic outlet syndrome which are based on the structures that are compressed. Therefore, thoracic outlet syndrome can be divided into 2 groups:
- Vascular Thoracic Outlet Syndrome (vTOS): which represents approximately 3% of cases and compression is of the vascular structures. vTOS is generally easier to define, diagnose and treat than nTOS (Sharp et al., 2001). There are 2 subtypes of vTOS which are:
- Venous TOS (venTOS): which involves compression of the subclavian or axillary vein and accounts for 2% of cases.
- Arterial TOS (aTOS): which involves compression of the subclavian or axillary artery and accounts for 1% of cases (Roos et al., 1987; Davidovic et al., 2003)
- Neurological Thoracic Outlet Syndrome (nTOS): represents approximately 97% of cases and compression is of the neural structures of the brachial plexus. Neurological TOS can be further divided into two groups, which are:
- True Neurological TOS (tnTOS): is associated with true neurological deficits (mostly muscular atrophy).
- Symptomatic TOS (sTOS): is associated with symptoms of TOS, however, there are no objective neurological, electro-physical or radiological abnormalities. This group is the largest group of TOS presentations, and remains the most controversial (Rayan, 1998; Lee et al., 2006). When talking about thoracic outlet syndrome – this is the group of patients you are most likely to encounter.
Aetiology of Thoracic Outlet Syndrome
Laulan et al. (2011) proposed four main causes of TOS which they have suggested can be interrelated. These are;
1. Congenital Abnormalities: these are often reported and can include:
- Boney Anomalies: such as a cervical rib or prolonged transverse process
- Fibrous Anomalies: including transversocostal and costocostal
- Muscular Anomalies: including scalenus anticus muscle and sickle-shaped scalenus medius
Whilst these abnormalities are often detected in those with true cases of TOS, they do not cause TOS, they are simply one of many predisposing factors.
2. Post-traumatic Causes: trauma, either macro or micro, seems to account for up to 2/3 of cases in some series (Roos, 1987; Ellison, 1994). Such causes include;
- Neck and shoulder trauma such as ‘whiplash’ injuries
- Upper limb trauma.
- Scalene muscle injury and subsequent fibrosis.
- Hypertrophic muscle morphotype of the cervicoscapular region
- Dropped Scapular morphotype or dyskinesis. This is discussed further below as a dropped scapula can lead to a dysfunction of the normal scalenus anterior muscle (Ellison, 1994, Watson et al., 2009).
4. Other Acquired Causes: whilst other causes are rare, they are important to be aware of, and they include:
- Tumours
- Hyperostosis
- Osteomyelitis
Assessment of Thoracic Outlet Syndrome
Unfortunately the diagnosis of TOS remains essentially clinical and is often one of exclusion with no objective sign or investigation being a specific predictor. Thus, it is essential that you undertake a thorough subjective and objective examination. Such a comprehensive upper body examination should include:
- Detailed body chart of all symptoms; including pain, neural symptoms, vascular symptoms
- Detailed history including instances of macro or micro trauma
- Aggravating and relieving activities and positions
- Postural alignment
- Active and passive ROM (of all relevant joints)
- Rotator cuff and glenohumeral joints tests
- Scapular dyskinesis assessment
- Neurological examination
- Peripheral nerve tests
- Manual muscle testing
- Special and provocation testing (discussed below)
The important thing to remember is that when assessing a patient with suspected thoracic outlet syndrome there are a large number of differential diagnoses that need to be excluded. Furthermore, your assessment will uncover information that will guide treatment and rehabilitation decisions (discussed below).
As you may expect the 2 types of TOS will vary slightly in clinical presentation, and as such they are discussed separately below.
Vascular TOS
Those with vascular symptoms are easier to assess and diagnose given the characteristic signs and symptoms. Subjectively, those with vascular TOS may report:
- Pain: often vague pain throughout the upper limb and hand.
- Other Symptoms: upper limb paraesthesia, stiffness, heaviness, temperature changes
- Aggravating Factors: overhead activities
- aTOS: may suffer ischemia related symptoms
- venTOS: may suffer swelling or venous engorgement
- Observation: classic TOS patients present with long neck and sloping shoulders (Kai et al., 2001)
- AROM: symptoms are typically reproduced/exacerbated with shoulder elevation
- Vascular Findings: including decreased pulse, ischemia, cyanosis, and oedema/swelling
- Special Vascular Tests: These include Adson’s Maneuver and Wright’s Test (shown in videos below). The aim of these tests is to obliterate distal pulses by causing a dynamic compression of the vascular vessels. However, the presence of dynamic compression is not synonymous with TOS, as it is detected in more than 50% of the general population (Roos, 1987, Laulan et al., 2011). Positive vascular tests, however, may help to guide the diagnosis.
Assessment of Neurological TOS
The vast majority of patients will present with nTOS, however, without any sign of true neurological deficits. This can make diagnosis very challenging! Lindgren (1997) developed a clinical index for TOS and suggested that patients should have at least three of the following four symptoms or signs.
- A history of aggravation of symptoms with the arm in an elevated position
- A history of paraesthesia originating from the spinal segments C8/T1.
- Supraclavicular tenderness over the brachial plexus
- A positive hands up abduction/external rotation or stress test.
Unfortunately clearly systematized symptoms are rarely present. Making our job more difficult the patient often reports vague, poorly defined, and inconsistent symptoms. Patients with sTOS are likely to report:
- Pain: upper limb, facial and cervicoscapular areas of pain
- Numbness in 66% of cases
- Decreased strength (55% of cases)
- Aggravating Factors: during activities requiring elevation of the arms (hanging up the washing, brushing one’s hair, etc.).
- Observation: shoulder girdle depression or “drooping” has been consistently observed (Kai et al., 2001)
- AROM: symptoms will be reproduced with shoulder flexion and abduction.
- Neurological Examination: signs of neurological deficit, essentially motor weakness (intrinsic muscles of the hand) should be investigated, but are seen rarely. Similarly, supraclavicular positive Tinel sign has a major diagnostic value, but is less often present.
- Manual Muscle Testing: you will likely find decreased strength in many shoulder girdle muscles (Watson et al., 2010).
- Scapular Assistance Technique: may reduce symptoms in those with “drooping” scapulae. If so, this is good indication for scapular retraining rehabilitation.
- Special Provocative Testing: the special tests for sTOS are quite sensitive but poorly specific.
- Roos Stress Test: technique is shown in the video below, this test has a fundamental diagnostic value provided it triggers the symptoms spontaneously experienced by the patient in less than one minute (Laulan et al., 2011).
- Elvey’s Test: involves taking the patient into 90 degrees of abduction/external rotation of the upper limb, wrist in extension, then the head is tilted to the contralateral side (Sanders et al., 2008). This tensions the peripheral nerves, and may be useful.
- Morley’s Sign: tenderness in the supra-clavicular fossa may have a diagnostic value when it is clearly asymmetrical and triggers distal pain (Laulan et al., 2011).
Roos Test Video
Investigations for Thoracic Outlet Syndrome
Laulan et al. (2011) suggest that none of the various complementary investigations are truly useful for the diagnosis of painful forms of TOS. However, it has also been suggested that the diagnosis of TOS must be a diagnosis of exclusion (Watson et al., 2009). Therefore, investigations should be utilised in the following cases:
- To exclude differential diagnoses, sinister or significant pathology
- In rare vascular forms
- In forms associated with true neurological deficits
- Prior to surgery
- Standard Radiographs/CT: may demonstrate bony anomalies such as a cervical rib or a prolonged C7 transverse process. However, as previously discussed, presence of such anomalies does not confirm the diagnosis of TOS.
- MRI: is of limited value for the diagnosis of TOS (Narakas et al., 1990), however, may be beneficial in excluding differential diagnoses (particularly sinister pathologies such as tumours).
- Static and Dynamic Vascular Examinations (Doppler ultrasound and angiography): useful in the presence of vascular clinical signs (discussed above)
- Electroneuromyography (ENMG): is usually normal, given the large proportion of symptomatic TOS patients. However, ENMG signs in favour of the diagnosis of nTOS are:
- Chronic partial denervation in intrinsic muscles of the hand
- Decreased amplitude of sensory evoked potentials of the ulnar nerve and motor evoked potentials of the median nerve
Differential Diagnoses for Thoracic Outlet Syndrome
As you may expect the potential list of differential diagnoses for TOS is lengthy. However, it is important to exclude many of the following to improve your clinical accuracy when attempting to diagnose TOS. The potential list (not exhaustive) includes;
- Cervical pain
- Tunnel syndromes
- Degenerative disease of the upper limb
- Upper limb tendinopathies
- Non-compressive central and peripheral neurological disease
- Rotator cuff syndrome
- Pancoast syndrome
- Radiation-induced brachial plexopathy
- Parsonage-Turner syndrome
- Syringomyelia
- Multiple sclerosis
- Amyotrophic lateral sclerosis (Laulan et al., 2011; Watson et al., 2009)
Conservative Physiotherapy Management
As alluded to throughout this article, treatment strategies for TOS remain highly controversial. However, it has been suggested that correctly conducted rehabilitation can provide prolonged relief of symptoms in about 2/3 of patients (Laulan et al., 2011). Good news, hey?
A Few General Treatment Caveats
There are a few general treatment caveats for the management of those with TOS, and this includes:
- All patients are individuals, and should be treated as such. These suggestions are by no means a recipe.
- Treatment must be based on assessment findings. If you are not assessing… you are just guessing!
- In all patients with TOS the therapist must always warn the patient to be on the alert for any alteration or aggravation in symptoms. Alteration of the scapula position may potentially exacerbate symptoms in TOS.
Generally, conservative management is accepted as the first form of management (Sharp et al., 2001). However, surgery is usually required for aTOS since there is often a structural lesion demonstrated. The decision for venTOS may be more difficult in the absence of bony structures responsible for compression. Initially, there may be a trial of conservative management (with surgical decompression performed if unsuccessful) including:
- Thromboembolytic Therapy
- Physiotherapy strategies (as discussed below)
- Symptom monitoring (Laulan et al., 2011).
As you have just read thoracic outlet syndrome is frequently multifactorial in its aetiology, and therefore successful treatment will likely target these factors. Accordingly, treatments will likely follow the identified issues in your thorough assessment. Treatments that you may find beneficial may include:
- Cervical mobilisation techniques
- Thoracic mobilisation techniques
- First rib mobilisation techniques
- Massage or myofascial tehniques – aimed at scalenes/pectoral muscles/scapular depressors. You willl find some beneficial techniques highlighted in our post on Treating Scapular Dyskinesis.
- Stretches: including scalene and pectoral muscles
- Neuromeningeal treatment techniques
- Supportive taping
- Postural re-education drills – important given the high frequency of postural issues identified
- Shoulder (including rotator cuff) and scapular strength and neuromuscular training exercises. These exercises are aimed at correcting the “Drooped Shoulder” postures/mechanics seen in may sTOS patients (Watson et al., 2010). Given that this is very important and there is a large range of treatment options/prescriptions in this area – I would urge you to seek out the brilliant paper by Watson et al. (2010)!
The aforementioned paper also states that improvements are regularly seen in those with sTOS, however, others make no improvement past platueas and discontinue trreatment. The authors suggest that if benefit are to be gained from the rehabilitation program then subjective and objective indicators of improvement should be seen within 6 – 12 weeks of initiating treatment (Watson et al., 2010).
Surgical Management of Thoracic Outlet Syndrome
As stated above, vTOS generally requires surgical treatment. The surgical techniques usually involves decompression of the thoracic outlet with removal of the cervical rib (if present) and/or first rib excision together with associated muscles and other soft tissue structures as indicated (Laulan et al., 2011).
With reference to nTOS surgery remains very controversial, even in relation to the various techniques (Riddell & Smith, 1986).
- Supraclavicular Scalenectomy: appears to be associated with a lower success rate (Gockel et al., 1994). However, a cervical approach is especially indicated for resection of a superficial cervical rib.
- Transaxillary Resection of the First Rib: an effective procedure provided all nervous and vascular structures are completely released. However, this surgery is difficult and not devoid of certain risks with a high morbidity (Laulan et al., 2011).
What Are Your Thoughts?
What is your experience working with patients with thoracic outlet syndrome? Hard to diagnose… a killer to treat? Be sure to let me know in the comments or catch me on Facebook or Twitter.
Promote Your Practice: Are you a physiotherapist or physical therapist looking to promote your own clinic, check this out.
Photo Credit: Keith Allison
References
Davidovic LB, Kostic DM, Jakovljevic NS, Kuzmanovic IL, Simic TM. Vascular thoracic outlet syndrome. World Journal of Surgery 2003;27(5):545–50.
Ellison DW, Wood VE. Trauma-related thoracic outlet syndrome. J Hand Surg. 1994;19B:424–6
Gockel M, Vastamaki M, Alaranta H. Long-term results of primary scalenectomy in the treatment of thoracic outlet syndrome. J Hand Surg. 1994;19B:229–33.
Kai Y, Oyama M, Kurose S, Inadome T, Oketani Y, Masuda Y. Neurogenic thoracic outlet syndrome in whiplash injury. Journal of Spinal Disorders 2001;14(6):487–93.
Laulan J, Fouquet B, Rodaix C, Jauffret P, Roquelaure Y, Descatha A. Thoracic outlet syndrome: definition, aetiological factors,diagnosis, management and occupational impact. J Occup Rehabil 2011;21:366–373
Lindgren KA, Oksala I. Long-term outcome of surgery for thoracic outlet syndrome. American Journal of Surgery 1995;169(3):358–60.
Lindgren KA. Conservative treatment of thoracic outlet syndrome: a 2-year followup. Archives of Physical Medicine and Rehabilitation 1997;78(4):373–8.
Mackinnon SE, Novak CB. Clinical commentary: pathogenesis of cumulative trauma disorder. J Hand Surg. 1994;19A:873–83.
Narakas AO. The role of thoracic outlet syndrome in the double crush syndrome. Ann Chir Main. 1990;9:331–40.
Ranney D. Thoracic outlet: an anatomical redefinition that makes clinical sense. Clinical Anatomy 1996;9(1):50–2.
Riddell DH, Smith BM. Thoracic and vascular aspects of thoracic outlet syndrome. Clin Orthop. 1986;207:31–6.
Rayan GM. Thoracic outlet syndrome. Journal of Shoulder and Elbow Surgery 1998;7(4):440–51.
Roos DB. Congenital anomalies associated with thoracic outlet syndrome. Am J Surg. 1976;132:771–8.
Roos DB. Thoracic outlet syndromes. Am J Surg. 1987;154: 568–73.
Sanders RJ, Hammond SL, Rao NM. Thoracic outlet syndrome: a review. Neurologist. 2008;14:365–73.
Sharp WJ, Nowak LR, Zamani T, Kresowik TF, Hoballah JJ, Ballinger BA, et al. Longterm follow-up and patient satisfaction after surgery for thoracic outlet syndrome. Annals of Vascular Surgery 2001;15(1):32–6.
Watson L, Pizzari T, Balster S. Thoracic outlet syndrome part 1: Clinical manifestations, differentiation and treatment pathways. Manual Therapy 2009;14:586–595
Watson L, Pizzari T, Balster S. Thoracic outlet syndrome Part 2: Conservative management of thoracic outlet. Manual Therapy 2010;15:305-314
Wright D, Jennings PR. Thoracic outlet syndrome. Journal of the American Academy of Physician Assistants 2005;18(5):57–8.
Yanaka K, Asakawa H, Matsumaru Y, Kujiraoka Y, Nose T. Diagnosis of vascular compression at the thoracic outlet using magnetic resonance angiography. European Neurology 2004;51(2):122–3.
Related Posts