Introduction
Many of the world’s sports physical therapists and physiotherapists spend their weekends at sporting events around the world. Unfortunately, many of us do not have the support of a huge medical team around us, such as that available to James Sutherland at Wallabies games. Therefore, we are often the most highly trained “medical” staff at any given event, and when it comes to injured athletes the buck stops with us. This means we require knowledge on a variety of conditions that may not be “sports” injuries and many abdominal injuries may fall outside the expertise of a physio.
Background Information
Abdominal trauma and injuries are quite rare in many sports (Ryan, 1999). However, such infrequency of serious abdominal trauma means that serious, albeit rare, conditions are often under-, or worse, undiagnosed. This is because the sports medicine professionals rarely encounter such presentations, and clinical suspicion may be quite low (Barret & Smith, 2012). It is therefore imperative that sports physiotherapists and physical therapists have an awareness of abdominal anatomy, injuries and appropriate management. This is particularly important for those therapists that work closely with sports that have been associated with abdominal trauma. These are often high velocity and contact sports and include:
- Football
- Skiing
- Motorcycle Events
- Cycling and Mountain Biking
- Fencing
- Equestrian (Ryan 1999; Barret & Smith, 2012)
-
Anatomy of Abdominal Injuries
As we will all be aware from our anatomy days – the abdomen is a relatively unprotected area with no bony protection. It is reliant upon the soft tissues of the abdominal wall to protect against trauma, and is therefore susceptible to trauma (Barret & Smith, 2012). Moore (2006) suggest the anatomy of the abdomen consists of: Muscles and Fascia:
- Rectus Abdominis
- Internal Oblique
- External Oblique
- Transversus Abdominis
- Pyramidalis (remember him?)
Organs:- Stomach
- Small Intestine
- Colon
- Appendix
- Liver
- Gallbladder
- Pancreas
- Spleen
- Kidneys
Lower Abdominal/Pelvic Organs
- Urinary Bladder
- Uterus, Fallopian Tubes and Ovaries in Women
Potential Abdominal Injury Presentations
There are many potential abdominal injuries that you may have to assess on the sideline. The following list is not exhaustive but will give a general idea of some differential diagnoses and should serve to increase your clinical suspicion of serious abdominal injuries. It is based on the clinically useful article written by Barrett and Smith (2012).
Abdominal Muscle Injury- This includes strain and contusion
- Mechanism: direct blow to the abdomen or stretch/contraction injury
- Symptoms: abdominal pain
- Action Required: these injuries may be treated via regular contusion or muscle injury protocols. Medical referral is required if there are signs of other significant injury.
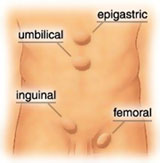
Hernia- Mechanism: increase in abdominal pressure – often due to muscular contraction or external force
- Symptoms: abdominal/groin pain
- Objective Signs: tenderness/palpable mass at herniation site (either the femoral ring or inguinal canal – see image below), pain with abdominal contraction
- Action Required: medical referral
Sports Hernia (Athletic Pubalgia)- If you are not familiar with this condition, check this out.
Solar Plexus Syndrome (Winded)- Mechanism: direct blow to the ‘solar plexus’ or the stomach resulting in temporary paralysis of the diaphragm
- Symptoms: acute difficulty breathing and distress
- Action Required: attempt to calm the athlete as the symptoms should resolve quickly. Crouching or raising knees may help resolve symptoms more quickly. Medical referral is required if there are signs of other injury or symptoms do not resolve within 10-15 minutes.
Bladder Rupture- Mechanism: direct blow to distended bladder
- Symptoms: abdominal pain, difficulty urinating
- Objective Signs: haematuria, abdominal rigidity
- Action Required: medical referral
Contused/Ruptured Kidney- Mechanism: direct blow to lower back/kidney
- Symptoms: flank/lower back pain, nausea, symptoms of shock (coldness, dizziness, weakness)
- Objective Signs: haematuria, abdominal rigidity and guarding, signs of shock (low BP, tachycardia, tachypnoea, cold clammy skin)
- Action Required: immediate medical referral
Intestinal Damage/Bowel Perforation- Mechanism: direct blow to abdomen
- Symptoms: abdominal pain, changes in bowel function/bloating
- Objective Signs: local tenderness, systemic symptoms including temperature and BP changes
- Action Required: immediate medical referral
Liver Trauma- Mechanism: direct blow to abdomen – especially right side
- Symptoms: abdominal pain, nausea, symptoms of shock (coldness, dizziness, weakness)
- Objective Signs: blood in vomit, faeces, or urine, abdominal rigidity and guarding, signs of shock (low BP, tachycardia, tachypnoea, cold clammy skin)
- Action Required: immediate medical referral
Spleen Ruptures
- Mechanism: direct blow to abdomen
- Symptoms: abdominal pain, symptoms of shock (coldness, dizziness, weakness)
- Objective Signs: local tenderness, systemic symptoms and signs of shock (low BP, tachycardia, tachypnoea, cold clammy skin)
- Action Required: immediate medical referral
The Kind Of Crashes That Cause These Abdominal Injuries
Indications for Medical/Hospital Referral
As suggested above, many abdominal injuries are not serious and do not require urgent medical referral. This will reflect what you are likely to see in the sideline setting. However, it is important to maintain a high clinical suspicion of significant or serious abdominal injury when assessing these athletes. If you are trying to decide when to refer your athlete on for further evaluation, the following indicate the need for immediate medical referral:
- All penetrating abdominal injuries
- Systemic symptoms – temperature and blood pressure changes
- Signs or symptoms of shock
- Blood in urine, feces or vomit
- Abdominal rigidity or muscle guarding
- Positive rebound tenderness (see video below)
- Worsening symptoms/objective signs
- If you’re not sure… no-one was ever sued because they did refer on (you don’t to be the therapist who didn’t refer a potentially life threatening injury on – although I’m not trying to scare you).
What Are Your Thoughts?
Have you ever assessed or managed an acute abdominal injury on the sidelines? I would love to hear about your experiences! So be sure to let me know in the comments or catch me on Facebook or Twitter.
Promote Your Clinic: Are you a physiotherapist or physical therapist looking to promote your own clinic, check this out.
References
Barrett C, Smith D. Recognition and management of abdominal injuries at athletic events. The International Journal of Sports Physical Therapy 2012;7(4):448
Diamond, D. Sports-related abdominal trauma. Clin Sports Med. 1989;8(1):91-9. Moore KL, Dalley AF, Agur AMR, & Moore ME. (2006). Clinically oriented anatomy (5th edition.). Baltimore, Maryland: Lippincott Williams & Wilkins
Ryan JM. Abdominal injuries and sport. British Journal of Sports Medicine 1999;33:155–160
Photo Credit: WikiCommons, Mikael Häggström via Wikimedia Commons. naotakem
Related Posts
Comments










nice article and important topic to be considered.
I had a cricketer with an acute abdominal strain during practice session. thou based on TOTAPS was easily able to establish the diagnosis and and got the confirmation with radiological investigation. I would completely agree with you on the referral part, its an important and can make a significant impact on injury management.