Introduction
The use of ultrasound therapy is widespread in sports physiotherapy and physical therapy practice (Khanna et al., 2009). In most cases it is used as an adjunctive therapy to other forms of treatment and rehabilitation. This, unfortunately, is in the absence of well-designed clinical trials demonstrating any significant improvement in human function. Now, this site does not really discuss the various forms of electrophysical agents and their potential role in the management of athletes, however, I would love to open a can of worms. This article will discuss recent research on low intensity pulsed ultrasound for the management of soft-tissue injuries.
Low Intensity Pulsed Ultrasound For Soft Tissue Injuries
A study published in the British Medical Bulletin by Khanna and colleagues (2009) evaluated the evidence for use of low intenstiy pulsed ultrasound (LIPUS) in soft tissue injuries. This article included studies with both animal and human participants and also in vivo and in vitro conditions. In summary, the review found the following results.
Intervertebral Disc. Ultrasound therapy had the following effects on nucleus pulposus material:
- Increased IVD cell proliferation and matrix synthesis
- Increased proteoglycan synthesis; which increased water uptake and may regress herniation
- Induced macrohpage migration; which may increase remodelling
- Increased collagen synthesis (16-19%) (Miyamoto et al., 2005)
Ligament. Ultrasound therapy was shown to have:
- Accelerated ligament healing
- Accelerated rat medial collateral ligament injury healing (Takakura et al. 2002; Sparrow et al., 2005).
Cartilage. Ultrasound therapy was shown to have the following effects on cartilage defects:
- Significantly improved full-thickness osteochondral defects with reference to both morphologic features and histologic characteristics of repaired cartilage.
- Enhanced the healing of cartilage defects in vivo.
- Cartilage healing assisted with LIPUS produces fewer degenerative changes in the long term, as compared with controls. (Cook et al., 2001).
Tendon. The 2009 review found that therapeutic ultrasound has been found to have no effect over and above placebo on tendon healing (Khanna et al., 2009). However, this may be contradicted by some brand new research discussed below.
New Research on Tendon Healing and Ultrasound Therapy
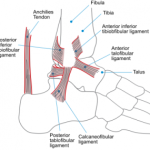
Junior et al. (2011) randomised 28 rats with surgically induced calcaneal tendon injuries into 2 groups, a control and a LIPUS groups. The experimental group underwent 28 consecutive days of low intensity pulsed ultrasound therapy, starting on the first postoperative day. The parameters and dosage where as follows:
- 2 W of irradiation intensity applied to an effective radiation area (ERA) head of 3.8 cm2
- 16-Hz frequency
- Pulsed 20% sonication periods
- Time: 5 minutes
- SATA = 0.1 W/cm2
- SAI = 0.52 W/cm2
- Subaquatic delivery technique
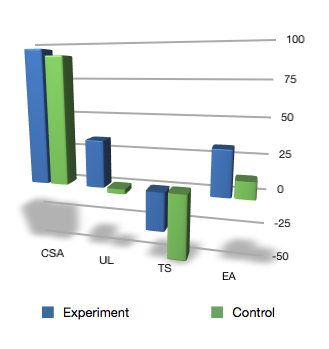
Following the experiment period the results were analysed. To account for differences in animals the results were normalised to the uninvolved limb, and therefore, each animal served as their own control. The study examined outcomes variables of cross-sectional area (CSA), ultimate load (UL), tensile strength (TS), and energy absorption (EA). The results are demonstrated graphically below, and are given as the mean percentage greater than the uninvolved side:
Thus, you can see the the experimental LIPUS groups consistently performed better on all outcomes, and therefore the LIPUS has improved the biomechanical properties of the tendon.
So does that mean we should utilise ultrasound therapy for all our tendon pathologies?
My Beef With Ultrasound Therapy
There a quite a few limitations in the ultrasound literature, particularly as it applies to general clinical practice. Whilst there are the obvious issues of in vitro and animal studies, that is the requirement for validation in vivo in human subjects. It is also necessay to question do these changes at a molecular and biochemical level translate to clinically relevant improvements in function? Additionally, there are the mechanisms of “induced” injuries which frequently do not mirror the mechanism of injury seen in our sports physiotherapy clinics (Junior et al., 2011).
I also see the prescribed dosages as an issue. These studies frequently utilise daily applications of the ultrasound therapy. Whilst this is clearly achievable in the realm of elite sports physiotherapy, this is generally not an option for the general sporting population and widespread physiotherapy/physical therapy practice. This is echoed in the review by Khanna (2009) who suggests the literature is deficient on the economical benefits of LIPUS on soft-tissue healing.
Furthermore there is a clear issue of time here. If you have a 15-30 minutes consultation with your athlete (the norm for many private practices), would you elect to up to a third of their time with you on ultrasound therapy? Do you have better tools in your sports physiotherapy toolbox that you could aim at this athlete? Whilst this is very clearly a decision for you to make, based on the evidence provided in the literature as well as an individual case basis, I feel the question is worth asking.
What Are Your Thoughts?
I would love to know what your thoughts are on the use of ultrasound therapy. Please leave a comment below and answer any of my rhetorical, implied or simply unasked questions. Alternatively, let us know of your victories and losses, trials and tribulations all as they apply to ultrasound therapy.
References
Cook SD, Salkeld SL, Popich-Patron LS, Ryaby JP, Jones DG, Barrack RL (2001) Improved cartilage repair after treatment with low-intensity pulsed ultrasound. Clin Orthop, 391, 231 – 243
Junior SLJ, Camanho GL, Bassit ACF, Forgas A, Ingham SJM, Abdall RJ. Low-intensity pulsed ultrasound accelerates healing in rat calcaneus tendon injuries. J Orthop Sports Phys Ther 2011;41(7):526-531
Khanna A, Nelmes RT, Gougoulias N, Maffulli N, Gray J. The effects of LIPUS on soft-tissue healing: a review of literature. Br Med Bull. 2009;89:169-182.
Miyamoto K, An HS, Sah RL et al. (2005) Exposure to pulsed low intensity ultrasound stimulates extracellular matrix metabolism of bovine intervertebral disc cells cultured in alginate beads. Spine, 30, 2398–2405.
Sparrow KJ, Finucane SD, Owen JR, Wayne JS. (2005) The effects of low-intensity ultrasound on medial collateral ligament healing in the rabbit model. Am J Sports Med, 33, 1048–1056.
Takakura Y, Matsui N, Yoshiya S et al. (2002) Low-intensity pulsed ultrasound enhances early healing of medial collateral ligament injuries in rats. J Ultrasound Med, 21, 283–288.
Related Posts
Comments








I would agree 100%. Studies are often animal studies and the results show changes at tissue level, but limited to no study shows change in functional status (especially considering time and money could be spent better with other treatments).
I will say it can have a pretty significant placebo effect with some people based on their beliefs about US. But this is not reason to use it, it is an opportunity to educate about placebo.
Thanks for the response Kory. As you know, there are significant placebo responses for many of our therapies. Thus the need for some well designed and placebo controlled studies!
thanks for your thoughtful summary of the situation of clinical use of ultrasound. Physio and other sports injury specialists will benefit from more accessible discussions like this one.
First, since you asked, and correct me please if I am wrong; I think there is a typo in the paragraph (My Beef). I interpret your meaning as in vivo, not in vitro human, as written.
Next – and I don’t want to promote someones product here – there are cost effective means of letting your patients have therapeutic ultrasound on a daily basis. It is doable.
And thanks once again (whomever you are) for beating the drum in favor of electrophysical agents generally in sports physio. I, for one, am right behind you. Cheers
Thank Cath, and yes I have fixed up the article re: in vitro! Interesting you bring up the home ultrasound options, as they have become more portable and affordable for home use, I will mention a product (http://www.ultralieve.com.au/) if readers are interested. I appreciate your interest and feedback!
Kia Ora,
With regards to the type of studies being carried out, I agree that daily application is not so clinically relevant to the wider population.
I guess the next step is to carry out a study utilising ultrasound 2-3 times weekly on human subjects measuring functional benefits…
I appreciate the suggested use of home ultrasound, but again, is the research convincing enough to purchase these or will 2-3 sessions a week be as functionally beneficial?
Great comment and point Emma, and I suppose the simple answer is that we need the research to find out. Until then we wait or extrapolate… Thanks again.
I still use ultrasound on occasion for soft tissue injuries on all parts of the body including ankle, knee, shoulder, elbow, cervical and lumbar spine.
But we and a number of other high profile physios in Australia and New Zealand have been using a new neuromagnetic device called Q magnets. They are a quadrapolar magnet that introduces magnetic field gradients for which there needs to be much more research, but there has been encouraging animal and invitro studies and the odd RCT that can be seen on this page.
http://www.qmagnets.com/magnetic-therapy-relevant-research.php
Your post got me thinking, and why I think it’s relevant is that while ultrasound requires a relatively large block of one-on-one patient time to deliver a therapeutic dose. Adjunct therapies such as Q magnets are relatively inexpensive and take only a few minutes to apply with sports tape and the patient walks out of the clinic and has treatment on the area 24/7 until I see them again.
Sometimes they completely desensitise sensitised nerves and often times where I would normally expect the patient to be recovery wise in a week, they reach these markers in a few days.
Thanks for your input Dianne. I must say I have little experience with these quadrapolar magnets, but you have certainly got me interested! Thanks again!
I saw one of those Ultrasounds at a patients house. The instructions said turn it one then put it on the problem area. I would suggest that the crystal is not going to last for very long so I doubt they are getting US anyway.
@ Helen… Correct me if I’m wrong, but I don’t think the treatment heads of the Ultralieve US units are made of quartz crystal. I think that’s partly how the keep the costs of the units down?
Although I would advocate having the treatment head in contact with the skin before turning it on – even if it’s just to maintain good practice!
I agree with some of the hesitations outlined above. Small sample sizes, animal studies, and dose frequencies that do not represent realistic clinical limitations. My experience here is that there is quite a placebo effect (I think most of us have had the experience of working as a junior physio, turning the noisy timer up on one of the older machines but forgetting to turn the intensity up, only for your client to return telling you how great the ultrasound made them feel!) While I readily accept that there is a placebo effect for many of the treatments that we use, I have found that there is almost always something better that I can do with my hands or through exercise that provides superior results
want to know that when ultrasonography is done for soft tissue injury condititionsthe report gives hypoechoic area highly vascular area.is there any research article of therapeutic ultrasound which gives dosimetry for the diff erent scenarios of the tissues such as hypoechoeic or hyper vascular areas
I think that with any therapy, there can be any number of theories backed up by physiological evidence to validate its use- however if the therapy is no more effective than placebo, let alone other effective therapies that can be applied what does it matter? I am a chiropractor and there are lots of articles on things like manipulation increasing Immunoglobulin production but what does that mean for my patients clinically? Nothing!
I feel that research in manual therapy needs to be lead much more by clinical outcomes rather than laboratory outcomes.
All those comments and suggestions mentioned seem to be relevant, though i disagree with some. Anyway, i think ultrasound seem to have a history of scholars and researchers stating lack of scientific evidence about its efficacy. Those utilizing it base their practice on experiences and opinion. This is the reason why i decided to take this topic for my research: A Study to examine the effectiveness of US therapy in acute soft tissue sports injury management. This research is a per-requisite of under graduate study. I hope this research will turn out well for me, and I’ll be able to abstract answers for my question, “is US therapy effective for soft tissue injury?” It’s a pretty interesting therapeutic modality.
Thanks for the comment, and best of luck with your research Debbie!
Now, I’m not a doctor or physical therapist, but my dad has used his own at home ultrasound machine on a few injuries and swears by it, saying he healed a lot faster. However, I hurt my foot about 3 months ago and even after 5 weeks in a boot and on crutches my foot hasn’t improved. I tried this ultrasound machine of his night before last and today, my foot has hurt more than it has in at least a week. That goes completely against using it to cut pain when it increases it. It was for 15 minutes on the highest setting (what he said to do) and my foot was already swollen for the previous couple months before doing this. I don’t know if this helps you all, but I hope it does. I know I’m trying to learn more about it as well.